Factors associated with depression and anxiety in nutritionists in the COVID-19 pandemic
DOI:
https://doi.org/10.17765/2176-9206.2023v16n4.e11845Keywords:
COVID-19, Anxiety, Depression, Suicidal Ideation, NutritionistsAbstract
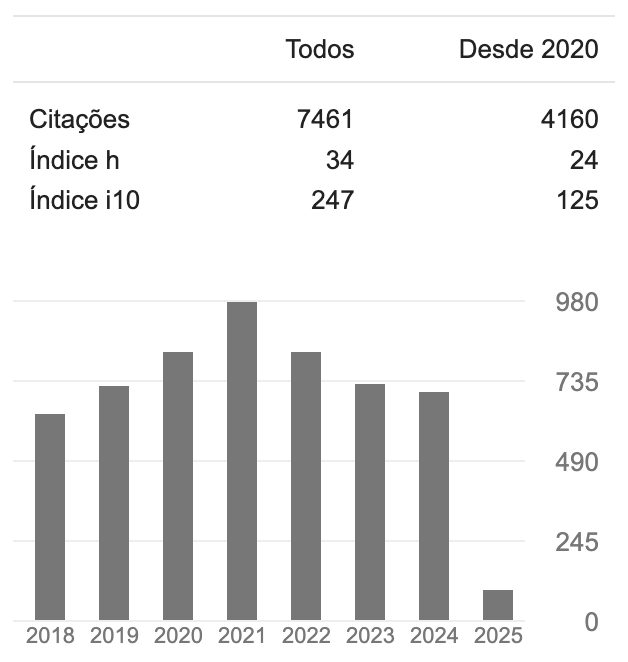
The objective was to investigate the factors associated with depression and/or anxiety and depression in nutritionists during the COVID-19 pandemic. Cross-sectional study with the application of the GAD-7 and PHQ-9 scales. 1,018 participated, of which 60.2% showed positive screening for depression and/or anxiety, with a greater strength of association for very frequent conflicts in relationships (OR = 11.11; 95%CI 6.61;18.67), use of pain medication (OR = 7.42; 95%CI 4.67;11.79) and always thinking about the pandemic (OR = 6.5; 95%CI 4.14;10.32). Not being under psychotherapeutic treatment (OR = 0.39; 95%CI 0.27;0.560) and not using psychotropic medication (OR = 0.40; 95%CI 0.26;0.60) were associated with lower odds of positive screening. This study results in epidemiological knowledge applicable to surveillance, prevention and control of anxiety and depression among nutritionists.Downloads
References
1. World Health Organization. Coronavírus disease (COVID-19) pandemic. [Internet] 2019 [cited 2021 Dec 19]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019
2. Oliveira TC, Abranches MV, Lana RM, (In)Segurança alimentar no contexto da pandemia por SARS-CoV-2, Cad Saúde Pública. 2020;36(4):e00055220. doi: http://dx.doi.org/10.1590/0102-311X00055220
3. Ozamiz-Etxebarria N, Dosil-Santamaria M, Picaza-Gorrochategui, M, Idoiaga-Mondragon N. Niveles de estrés, ansiedad y depresión en la primera fase del brote del COVID-19 en una muestra recogida en el norte de España. Cad Saúde Pública. 2020;36(4):e00054020. doi: https://doi.org/10.1590/0102-311X00054020
4. Liu Y, Sandmann FG, Barnard RC, Pearson CAB, Pastore R, Pebody R, et al. Optimising health and economic impacts of COVID-19 vaccine prioritisation strategies in the WHO European Region: a mathematical modelling study. The Lancet Regional Health – Europe. 2022;12:100267. doi: https://doi.org/10.1101/2021.07.09.21260272
5. Almeida WDSD, Szwarcwald CL, Malta DC, Barros MBDA, Souza Júnior PRBD, Azevedo LO, et al. Mudanças nas condições socioeconômicas e de saúde dos brasileiros durante a pandemia de COVID-19. Rev Bras Epidemiol. 2021;23:e200105. doi: https://doi.org/10.1590/1980-549720200105
6. Liu N, Zhang, F, Wei C, Jia Y, Shang Z, Sun L, et al. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: Gender differences matter. Psychiatry Res. 2020;287:112921. doi: https://doi.org/10.1016/j.psychres.2020.112921
7. World Health Organization. Depression and Other Common Mental Disorders – Global Health Estimates. [Internet] 2017 [cited 2021 Mar 31]. Available from: https://apps.who.int/iris/bitstream/handle/10665/254610/WHO-MSD-MER-2017.2-eng.pdf?s
8. Barros MBA, Lima MG, Malta DC, Szwarcwald CL, Azevedo RCS, Romero D, et al. Report on sadness/depression, nervousness/anxiety and sleep problems in the Brazilian adult population during the COVID-19 pandemic. Epidemiol Serv Saúde. 2020;29(4):e2020427. doi: https://doi.org/10.1590/s1679-49742020000400018
9. Teixeira CFS, Soares CM, Souza EA, Lisboa ES, Pinto ICM, Andrade LR, et al. A saúde dos profissionais de saúde no enfrentamento da pandemia de Covid-19. Cienc Saúde Coletiva. 2020;25(9):3465-74. doi: https://doi.org/10.1590/1413-81232020259.19562020
10. Prado AD, Peixoto BC, Silva AMB, Scalia LAM. A saúde mental dos profissionais de saúde frente à pandemia do COVID-19: uma revisão integrativa. REAS. 2020; 46:e4128. doi: https://doi.org/10.25248/reas.e4128.2020
11. Sher L. The impact of the COVID-19 pandemic on suicide rates. QJM. 2020;113(10):707-12. doi: https://doi.org/10.1093/qjmed/hcaa202
12. Luceño-Moreno L, Talavera-Velasco B, García-Albuerne Y, Martín-García J. Symptoms of Posttraumatic Stress, Anxiety, Depression, Levels of Resilience and Burnout in Spanish Health Personnel during the COVID-19 Pandemic. Int J Environ Res Public Health. 2020;17(15):5514. doi: https://doi.org/10.3390/ijerph17155514
13. Liu Y, Chen H, Zhang N, Wang X, Fan Q, Zhang Y, et al. Anxiety and depression symptoms of medical staff under COVID-19 epidemic in China. J Affect Disord. 2021; 278:144-48. doi: https://doi.org/10.1016/j.jad.2020.09.004
14. Conselho Federal de Nutricionistas (CFN). [Internet]. [S.d.] [citado em 2022 dez 15]. Disponível em: https://www.cfn.org.br/
15. Moreno AL, Sousa D, Souza AMFLP, Manfro GG, Salum GA, Koller SH, et al. Factor structure, reliability, and item parameters of the brazilian-portuguese version of the GAD-7 questionnaire. Temas Psicol. 2016;24(1):367-76. doi: https://doi.org/10.9788/tp2016.1-25
16. Santos IS, Tavares BF, Munhoz TN, Almeida LS, Silva NT, Tams BD, et al. Sensibilidade e especificidade do Patient Health Questionnaire-9 (PHQ-9) entre adultos da população geral. Cad Saúde Pública. 2013;29(8):1533-43. doi: https://doi.org/10.1590/0102-311x00144612
17. Pierce M, Hope H, Ford T, Hatch S, Hotopf M, John A, et al. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry. 2020;7:883-92. doi: https://doi.org/10.1016/S2215-0366(20)30308-4
18. O'Connor RC, Wetherall K, Cleare S, McClelland H, Melson AJ, Niedzwiedz CL, et al. Mental health and well-being during the COVID-19 pandemic: longitudinal analyses of adults in the UK COVID-19 Mental Health & Wellbeing study. Br J Psychiatry. 2020; 21:1-8. doi: https://doi.org/10.1192/bjp.2020.212
19. Mrklas K, Shalaby R, Hrabok M, Gusnowski A, Vuong W, Surood S, et al. Prevalence of Perceived Stress, Anxiety, Depression, and Obsessive-Compulsive Symptoms in Health Care Workers and Other Workers in Alberta During the COVID-19 Pandemic: Cross-Sectional Survey. JMIR Mental Health. 2020;7(9):e22408. doi: https://doi.org/10.2196/22408
20. Bicalho PP, Lima CH, Davi JS. Da crise à pandemia: da letalidade como política às políticas editoriais de resistência. Arq Bras Psicol. 2020;2(1):3-7. doi: https://doi.org/10.36482/1809-5267.ARBP2020v72i2p.3-7
21. Liu CH, Zhang E, Wong GTF, Hyun S, Hahm HC. Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: Clinical implications for U.S. young adult mental health. Psychiatry Res. 2020; 290:113172. doi: https://doi.org/10.1016/j.psychres.2020.113172
22. Klimkiewicz A, Schmalenberg A, Klimkiewicz J, Jasińska A, Jasionowska J, Machura W, et al. COVID-19 Pandemic Influence on Healthcare Professionals. J Clin Med. 2021;19;10(6):1280. doi: https://doi.org/10.3390/jcm10061280
23. Gonçalves AMC, Teixeira MTB, Almeida JR, Gama CSL, Silva GA, Gamarra CJ, et al. Prevalência de depressão e fatores associados em mulheres atendidas pela Estratégia de Saúde da Família. J Bras Psiquiatr. 2018;67(2):101-9. doi: https://doi.org/10.1590/0047-2085000000192
24. Instituto de Pesquisa Econômica Aplicada. Retrato das desigualdades de gênero e raça. [Internet] 2011 [citado em 2021 dez 17]. Disponível em: https://www.ipea.gov.br/retrato/pdf/revista.pdf
25. Malta DC, Szwarcwald CL, Barros MBA, Gomes CS, Machado ÍE, Souza JPRB, et al. A pandemia da COVID-19 e as mudanças no estilo de vida dos brasileiros adultos: um estudo transversal, 2020. Epidemiol Serv Saúde. 2020;29(4):e2020407. doi: http://dx.doi.org/10.1590/s1679-49742020000400026
26. Guedes AC, Kantorski LP, Willrich JQ, Coimbra VCC, Wünsch CG, Sperb LCSO, et al. Online mental health care during the COVID-19 pandemic. Rev Bras Enferm. 2022;75 (Suppl 1):e20210554. doi: http://dx.doi.org/10.1590/0034-7167-2021-0554
27. Silva Júnior F, Monteiro C, Sales, J, Andrade S, Veloso L, Costa AP. Ideação suicida, consumo de bebidas alcoólicas e tabaco pelas mulheres. Rev Port Enferm Saúde Mental. 2021;25:69-82. doi: http://dx.doi.org/10.15309/17psd180206
28. Pereira AS, Willhelm AR, Koller SH, Almeida RMM. Fatores de risco e proteção para tentativa de suicídio na adultez emergente. Cien Saúde Colet. 2018;23(11):3767-77. doi: http://dx.doi.org/10.1590/1413-812320182311.29112016.
29. Iob E, Steptoe A, Fancourt D. Abuse, self-harm and suicidal ideation in the UK during the COVID-19 pandemic. Br J Psychiatry. 2020; 217:543-6. doi: https://doi.org/10.1192/bjp.2020.130
30. Pirkis J, John A, Shin S, Del Pozo-Banos M, Arya V, Analuisa-Aguilar P, et al. Suicide trends in the early months of the COVID-19 pandemic: an interrupted time-series analysis of preliminary data from 21 countries. Lancet Phychiatric. 2021;8(7):579-88. doi: https://doi.org/10.1016/S2215-0366(21)00091-2
Downloads
Published
How to Cite
Issue
Section
License
A submissão de originais para a revista Saúde e Pesquisa implica na transferência da Carta Concessão de Direitos Autorais, pelos autores, dos direitos de publicação digital para a revista após serem informados do aceite de publicação.A Secretaria Editorial irá fornecer da um modelo de Carta de Concessão de Direitos Autorais, indicando o cumprimento integral de princípios éticos e legislação específica. Os direitos autorais dos artigos publicados nesta revista são de direito do autor, com direitos da revista sobre a primeira publicação. Os autores somente poderão utilizar os mesmos resultados em outras publicações, indicando claramente a revista Saúde e Pesquisa como o meio da publicação original. Em virtude de tratar-se de um periódico de acesso aberto, é permitido o uso gratuito dos artigos, principalmente em aplicações educacionais e científicas, desde que citada a fonte. A Saúde e Pesquisa adota a licença Creative Commons Attribution 4.0 International.
A revista se reserva o direito de efetuar, nos originais, alterações de ordem normativa, ortográfica e gramatical, com vistas a manter o padrão culto da língua e a credibilidade do veículo. Respeitará, no entanto, o estilo de escrever dos autores. Alterações, correções ou sugestões de ordem conceitual serão encaminhadas aos autores, quando necessário. Nesses casos, os artigos, depois de adequados, deverão ser submetidos a nova apreciação. As opiniões emitidas pelos autores dos artigos são de sua exclusiva responsabilidade.