Effectiveness of online psychosocial interventions for reducing depression, anxiety, and stress: a quasi-experimental study
Efetividade de intervenções psicossociais online para a redução de depressão, ansiedade e estresse: estudo quase-experimental
DOI:
https://doi.org/10.17765/2176-9206.2024v17n1.12260Keywords:
Mental health, COVID-19., Psychosocial Support Systems, e-TherapiesAbstract
This study aimed to evaluate the effectiveness of online group psychosocial therapies in reducing symptoms of depression, anxiety, and stress during the COVID-19 pandemic. It was a quasi-experimental study, with the DASS-21 scale applied to participants of therapeutic groups (n=66) at two time points: pre- and post-therapies. By using the paired sample t-test, a comparison of the means of the scores found was made. The results indicated a reduction in symptoms with statistically significant differences between the means, considering p<0.01, and effect sizes ranging from small (0.20-0.49) to medium (0.50-0.80). The differences found suggest the effectiveness of online group psychosocial therapies as strategies for well-being, psychosocial support, matrix support, and expressive spaces in coping with the pandemic context, which can be replicated in other contexts and public health services.
Keywords: Mental health. COVID-19. Psychosocial Support Systems. e-Therapies.
INTRODUCTION
The COVID-19 pandemic has harmed mental health and psychological well-being globally. Population-based studies across various countries have reported mental health impacts, showing a high prevalence of anxiety, depression, stress, and changes in psychological well-being. Populations identified as being at greater vulnerability included women, students, non-white ethnicities, single individuals, the unemployed, and those at higher risk of infection1?7.
These early-pandemic studies highlighted the need for online psychosocial interventions to alleviate psychological distress. The Pan American Health Organization (PAHO) recommended the development of Mental Health and Psychosocial Support (MHPSS) strategies by health professionals, not necessarily psychologists, working in public health services and community structures. The main goal was to reduce the psychological suffering of people affected directly or indirectly by COVID-198.
In contexts of highly contagious disease outbreaks, psychosocial interventions that combine teaching coping strategies, relaxation techniques, cognitive-behavioral approaches, and spiritual techniques have shown positive effects on the health of various groups, including healthcare workers. These effects included promoting well-being and resilience, reducing psychological stress in children and adolescents, and increasing the sense of social commitment9-10.
A systematic review of 59 studies on the impact of the early stages of the COVID-19 pandemic on the mental health of healthcare professionals identified six studies describing psychosocial intervention implementations with no analysis of their effects. The authors pointed out the need to design and evaluate such actions to generate more evidence on these interventions11. In hospital settings, the analysis of social support, whether in-person or online, showed improvements in coping mechanisms for stress, sleep-related symptoms, depression, and anxiety, both for COVID-19-positive patients and for medical teams caring for infected patients12-13.
In general, the remote format of MHPSS strategies, especially for short- or medium-term online psychological support, results in improved connection and communication during social restriction periods, overcoming geographical boundaries. It also facilitates the sharing of experiences, serving as a way to alleviate fear and anxiety in dealing with this pandemic14-15.
Analysis of data from other studies, as the pandemic continued, showed the online environment to be promising for MHPSS interventions in various contexts. Individual and psychological care examples include: in Spain, an app-based intervention showed moderate symptom reduction for depression among participants16; in Germany, online psychotherapeutic interventions compared to face-to-face psychotherapy proved to be a useful tool, though not recommended as monotherapy17; and self-guided cognitive-behavioral therapies via readings and internet access links also showed a small but significant reduction in depression and anxiety symptoms in adults in Australia and the United Kingdom18. A narrative literature review analyzed six studies on Virtual Reality technology for individuals with mental disorders, revealing its effectiveness in improving users' sense of assistance and psychological presence during the pandemic19.
Less frequently, online group interventions were evaluated during the pandemic. In Greece, an online group positive psychological intervention effectively increased resilience, understanding of others' perspectives, positive emotion levels, and reduced negative emotions, with significant effects persisting post-intervention20. In Brazil, an online psychoeducation group led by a nurse and a psychologist for university students offered opportunities to improve self-awareness, emotional management, interpersonal relationships, empathy, and stress reduction. The remote setting was deemed comfortable for shy individuals or those who find face-to-face interactions challenging. Participants noted the lack of physical contact and potential academic overload as limiting factors, affecting the availability of self-care.
A systematic review of online group psychological interventions analyzed 24 articles from different countries and target audiences, showing improvements in psychological resources (resilience, empathy, life satisfaction, positive aspects) and reductions in pandemic?defined risk factors. Additionally, group interventions with participants having organic diseases showed decreases in pain, fatigue, and sleep disorders, and a reduction in psychopathological symptoms in patients with systemic sclerosis. Among the issues raised by the authors were questions about the adequacy and effectiveness of specific procedures for different population characteristics, the role of specific and nonspecific factors in comparing online and face-to-face groups, and the need for more detailed descriptions of intervention processes. Nonetheless, the results were encouraging for providing scientific evidence on the efficacy of online group interventions compared to face-to-face interventions22.
A meta-analysis of 10 studies on online psychological interventions with students from 7 American, 2 Asian, and 1 African universities found better efficacy in reducing stress and depression symptoms, especially in positive psychological interventions. The efficacy was maintained in follow-up assessments for depression symptoms, but not for anxiety. Due to high heterogeneity in the included studies, the authors suggest new studies should have greater control over variables such as trial setting, participant characteristics, outcome measures, ways of delivering psychosocial interventions, and trial procedures, as well as control group follow?up23.
Another systematic review and meta-analysis of 19 randomized clinical trials on multiple psychosocial interventions during the COVID-19 pandemic found greater efficacy in reducing symptoms of depression and insomnia, and less for symptoms of anxiety and stress. This study also referred to the heterogeneity of the studies as a limiting factor and pointed out another factor related to the limited number of articles available that met their inclusion criteria. According to the authors, many studies did not follow up on the effects of interventions or did not aim for data on the control group, making it difficult to determine the efficacy of the internet in psychosocial interventions for certain mental health problems24.
It is evident that most interventions are psychological in nature, conducted individually with a behavioral approach16-18, 22-23. Additionally, some were guided by therapists or self-guided through apps19, 24. Regarding efficacy, they presented, among other benefits already mentioned, control of depression, anxiety, and stress25-27. Thus, the pandemic context has expanded and stimulated scientific research and the creation of digital tools for healthcare promotion. However, there is still much to improve and explore regarding the use and study of such technologies28.
In this context, the e-Therapies Project was developed to offer and evaluate the effectiveness of psychosocial interventions as online therapeutic groups. This study aimed to answer the following question: “What is the effectiveness of the online psychosocial interventions carried out by the 'e-Therapies Project' in reducing symptoms of depression, anxiety, and stress in the population served?” Therefore, this study sought to evaluate the effectiveness of online psychosocial interventions in reducing symptoms of depression, anxiety, and stress during the COVID-19 pandemic.
METHODOLOGY
This is a quasi-experimental, pre-and-post study29, based on anxiety, stress, and depression symptom measurement scales, to evaluate online group psychosocial interventions performed through the e-Therapies Project. This project emerged during the COVID-19 pandemic because of the Action Research titled "Effectiveness of psychosocial e-therapies in coping with the COVID-19 pandemic," involving two public higher education institutions in Brazil and the support of the Bahia State Research Support Foundation (FAPESB), through the Support Program for Priority Research to the Unified Health System (PPSUS).
Utilizing the e-Therapies Project, four main modalities of online group psychosocial interventions were developed: well-being therapies aimed at promoting well-being via group interaction and directed activities; psychosocial support therapies, which work with care strategies to reduce symptoms of depression, anxiety, and stress; matrix support therapies that offer support and reflections on professional practices and their challenges; and expressive therapies that allowed the expression of feelings and emotions through writing, speech, and the arts. In total, distributed across the four modalities, the project developed 19 different online group psychosocial interventions, offered biannually during the years 2020 and 2021, using approaches such as: integrative community therapy, enneagram, life skills, caring for sleep quality, literary chat, therapeutic writing, and network dialogues - the latter for listening and matrix support of health care and social assistance networks workers30.
Each group intervention occurred in weekly or bi-weekly meetings, lasting about three months, totaling 8 to 12 meetings per group, with each session lasting between one and two hours. At least two professionals performed the mediation; they were from various health areas, active in mental health, namely: nursing, psychology, psychiatry, physical education, physiotherapy, nutrition, occupational therapy, and social assistance professionals. All of them received training to provide services through internet-based information and communication technologies using free digital platforms, in a synchronous manner and with the possibility of videoconferencing.
The "menu of offerings" of online psychosocial therapies was available on the project's specific website, with specifications of the group proposals, frequency, start dates and meeting forecasts, targeted audiences, as well as information about the mediators and their approaches. Interested individuals could access the registration form and indicate their choices.
The non-probabilistic sample consisted of 66 participants from the online intervention groups who met the following inclusion criteria: being over 18 years old; agreeing to participate in the research by signing the Informed Consent Form; and responding to the evaluation forms before and after the intervention. Those who responded to the evaluation form only at one time point and those who indicated participation in more than one e-therapy modality during the same period were excluded from the sample.
An online questionnaire adapted to Google Forms was utilized, taking approximately ten minutes to complete, containing sociodemographic data such as: gender, age group, color, children, occupation, income, education, religion, residence city, COVID-19 status, and reported health state. Additionally, they answered the 21 items of the Short Depression, Anxiety, and Stress Scale (DASS-21). This questionnaire was made available for self?application at two points: pre-therapy, considered in the first week of interventions, and post-therapy, in the final week of interventions.
The DASS-21 is a self-report scale featuring 21 items, adapted and validated for Brazilian Portuguese. Scores are assigned on a Likert scale, ranging from 0 (did not apply at all) to 3 (applied very much or most of the time), reflecting the participants' feelings over the last week. The instrument consists of three subscales: depression, anxiety, and stress. Scores for each subscale were summed and multiplied by 2 to obtain the final score, indicating the severity levels of symptoms31.
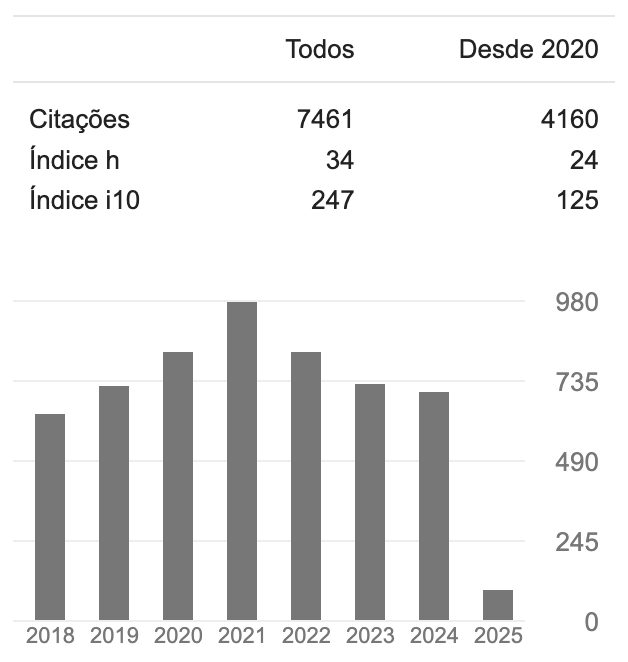
Data were initially analyzed using descriptive statistics, presented as mean and standard deviation for continuous variables, and absolute and relative frequencies for categorical variables. A posteriori power calculation was performed using G Power v. 3.1.9.4 software with the smallest effect size found in the study (dz=0.35), a 5% error, and n=66, resulting in an approximate power of 88%. Cronbach's Alpha Coefficient was used to evaluate the internal consistency (20) of the DASS-21 instrument in each of its dimensions, as well as the total score at pre- and post-therapy moments. The findings suggest reliability, as per Cronbach's coefficient analysis32, which varied between high (0.75-0.90) and very high (>0.90). Using the paired t?test, a comparison was made between the average scores from the DASS-21, for each dimension, and the total scores between pre- and post-therapy moments. The effect size (Cohen's dz) for comparing paired samples was calculated considering values small (dz=0.20-0.49); medium (dz=0.50-0.79); large (dz=0.80-1.19) and very large (dz ≥ 1.20)33. To assess the proportion of results regarding symptom severity levels, at pre- and post-therapy moments, the McNemar Test for related samples was used, recategorizing the DASS-21 into "expected levels" and "above expected levels," considering the scale's cutoff points: depression ≥ 10, anxiety ≥ 7, stress ≥ 1434. A significance level of 5% was adopted for all analyses, and the statistical package used was IBM SPSS Statistics for Windows, Version 25.0 (Armonk, NY: IBM).
The National Research Ethics Commission approved this study under the opinion number 4.063.178 and CAAE 31567220.51001.5526. To respond to the electronic questionnaire, all participants consented to their participation, through agreement with the Informed Consent Form (ICF) contained in the questionnaire.
RESULTS
In total, 309 responses were collected at the pre-therapy moment and 141 responses at the post-therapy moment. After applying the exclusion criteria, the sample consisted of n=66. Most participants were female (83.3%), and young adults aged 20 to 40 years (65.2%) without children (65.2%). Regarding race, 78.7% declared themselves as black, mixed race, and of indigenous origin. Of the participants, 69.7% lived in cities around one of the universities where the action research took place. The most frequent occupation reported was students (40.9%), mostly university students (36.4%), followed by health professionals (13.6%), teachers (12.1%), and 33.3% were distributed among other professions or unemployed. Altogether, 42.4% declared a family income of up to R$ 2,000.00. Considering the level of education, 63.6% have at least a higher education degree, and 77.3% reported having a religion (Table 1).
At the time participants started the e-therapies, 93.9% had not yet tested positive for COVID-19, and 28.8% had already been in quarantine or social isolation. The general health status was self-reported by 31.8% of participants as fair to very poor (Table 1).
Regarding participation in the offered online psychosocial therapy modalities, the distribution of choices among participants was 18.2% for well-being promotion therapies; 54.5% for psychosocial support therapies; 10.6% for matrix support therapies; and 16.7% for expressive therapies. Comparisons between the average scores at pre- and post-therapy moments are presented in Table 2, according to the DASS-21 dimensions and the total score. Statistically significant differences (p<0.01) were observed in the average scores across all dimensions, with effect sizes ranging from small (0.20-0.49) to medium (0.50-0.80). There was a reduction in symptoms of depression and anxiety after the interventions, particularly with the largest effect size observed in the stress dimension.
Considering the frequencies of responses to the DASS-21 by levels of symptom severity, the comparison between pre- and post-therapy moments is demonstrated in Table 3. The exact McNemar test showed differences in the proportions of responses for the expected levels of symptoms and levels above expected, between the two evaluation moments in the dimensions of the DASS-21, with p<0.05 for each of them. However, when comparing the proportions to the total result, the difference was not statistically significant.
DISCUSSION
This study is among the few that evaluated the effectiveness of psychosocial therapies, created by multidisciplinary teams and offered as online therapeutic groups, in reducing symptoms related to depression, anxiety, and stress, during the COVID-19 pandemic period, as most studies in the literature focus on psychological interventions.
The findings suggest that online psychosocial therapies, applied weekly for about three months, served as psychosocial support, improving the mental health of the researched population. The differences in analyzed scores indicate an effect of these interventions in reducing symptomatology as measured by the DASS-21.
Regarding symptom severity levels, there was a shift from "expected levels" to "above expected levels" after the intervention. Although the differences in proportions considering the total result were not statistically significant, a higher number of individuals with expected symptom levels and a reduction in individuals with above expected levels were observed post?intervention in the dimensions of depression, anxiety, and stress.
These findings support other studies that evaluated online interventions offered during times of coping with psychological distress resulting from events like the COVID-19 pandemic, which were deemed feasible and important for mitigating its effects on people's mental health, especially in reducing symptoms of depression and anxiety35.
Results related to stress showed differences with a larger effect size, as found in the literature27. Only one meta-analysis that examined the efficacy of psychological support interventions for the general population and health professionals concluded there was a benefit in controlling depression and anxiety but reported an ambiguous effect for stress, without statistically significant values. It is worth noting that this study also included face-to-face interventions25, 27.
It was noted that the demographic profile of those seeking online therapy groups aligns with the literature findings. The highlights are on populations more vulnerable to psychological distress with a higher likelihood of severe symptoms of depression, anxiety, and stress during this period: women, young adults (18 to 40 years), without children, non-white, university students, and those with a family income below R$2,000.00, indicating low income. These data reveal the impact of gender, race, and social conditions on pandemic experiences36-37.
Concerning the reported occupations, there was participation from professionals throughout various fields, particularly health workers, who experienced an increased workload and thus greater exposure to COVID-19 contagion risk. The pandemic period heightened symptoms of depression, anxiety, and stress to varying degrees across different countries. Generally, post?traumatic stress levels were higher among these professionals, possibly one of the reasons they sought psychosocial support during this time38.
Similarly, teaching professionals sought support, already burdened by workload, facing significant challenges due to pandemic-induced work changes, which lead to high levels of depression, anxiety, and stress39.
The significant participation of university students in therapies might be because of extensive promotion within partner universities and the opportunity for emotional support amidst academic uncertainties, highlighting the psychosocial factors further compromising their mental health40.
Although most survey respondents had not contracted COVID-19 or been quarantined when starting therapies, pandemic-induced fear of these situations and self-reported fair and poor health suggest mental health impacts, as indicated by early pandemic studies with COVID?19 symptomatic individuals41.
The most sought-after therapies focused on psychosocial support and well-being promotion, likely due to their direct strategies for handling pandemic-aggravated anxiety and stress symptoms. Further research could help understand participant choices, motivation, adherence, and satisfaction with e-therapies, potentially improving their offerings.
The utilization of internet-based information and communication technologies was crucial for reaching the population when physical contact was hindered by enforced distancing measures. By reducing symptoms of stress, anxiety, and depression, online psychosocial interventions served as vital psychosocial support and care, facilitating connections and exchanges of experiences. These results align with studies20, 24, 42 showing online group interventions as a viable and effective mental health promotion strategy for public health services, aiming to improve access and quality of care. Thus, online interventions enable interaction between those needing support and those able to provide it, even beyond the pandemic context43, suggesting the benefit of targeted interventions for specific groups20.
This study also supports expanding roles in mental health care through a multidisciplinary approach, training professionals as online therapeutic group moderators, allowing diverse intervention types. It encourages developing apps for psychosocial support and detailed, continuous data collection on human behavior and health, like the Neuropesquisa App28, designed for studying mental health biomarkers. Therefore, digital tools could enhance mental health prevention and promotion actions.
However, access to communication devices and quality internet is not universal in the study country, presenting a public health challenge for low-income populations. Another access challenge is the need for digital technology education for populations struggling with existing tools. A study44 on digital training for older individuals provides strong evidence of education as a tool for the use of new technology by this group, potentially improving psychological life quality scores, particularly autonomy.
Finally, limitations of this study relate to the sample type, as the evaluated intervention was demand-driven, with participants enrolling based on interest and availability; lack of detailed sociodemographic data; no separate evaluation of each online psychosocial therapy, complicating effectiveness comparisons; findings only reflect self-reported symptoms; no investigation into additional strategies or treatments used alongside e-Therapies; and the absence of a control group.
CONCLUSION
This study confirmed the importance of psychosocial interventions in mitigating the adverse mental health effects of the COVID-19 pandemic's scale. The findings suggest that online psychosocial therapies, provided in groups by multidisciplinary mental health teams, reduce symptoms of depression, anxiety, and stress. These therapies serve as well-being promotion strategies, psychosocial and matrix support, and offer expressive spaces for coping with the pandemic context.
Despite its limitations, the study highlights the potential of expanding mental health therapeutic actions accessible from any distance through internet-based information and communication technology. These actions should target populations needing psychosocial support during challenging times, like the COVID-19 pandemic, and can be replicated in other settings, including public health services.
While online psychosocial therapies have proven to be an effective support, they should not be seen as the sole option, especially for more severe cases of depression, anxiety, and stress. Future studies are recommended to address the limitations of this study, enhancing the use of these strategies and gathering more evidence on their efficacy.
Downloads
References
Salari N, Hosseinian-Far A, Jalali R, Vaise-Rygani A, Rasoupoor S, Mohammadi M, et al. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis [Internet]. 2020 Jul [cited 2021 Dec 9];16(1):57. doi:10.1186/s12992-020-00589-w.
Shevlin M, McBride O, Murphy J, Miller JG, Hartman TK, Levita L, et al. Anxiety, depression, traumatic stress and COVID-19-related anxiety in the UK general population during the COVID-19 pandemic. BJPsych Open [Internet]. 2020 Oct [cited 2021 Dec 9];6(6):e125. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7573460/ doi:10.1192/bjo.2020.109
Luo Y, Chua CR, Xiong Z, Ho RC, Ho CSH. A Systematic Review of the Impact of Viral Respiratory Epidemics on Mental Health: An Implication on the Coronavirus Disease 2019 Pandemic. Front Psychiatry. 2020 Nov [cited 2021 Dec 9];11:565098. doi:10.3389/fpsyt.2020.565098.
Lobo LAC, Rieth CE. Mental health and Covid-19: an integrative literature review. Saúde debate [Internet]. 2022 June [cited 2022 Oct 22];45(130):885-901. doi: 10.1590/0103-1104202113024
Wong LP, Alias H, Md Fuzi AA, Omar IS, Mohamad Nor A, Tan MP, et al. Escalating progression of mental health disorders during the COVID-19 pandemic: Evidence from a nationwide survey. PLos ONE [Internet]. 2021 Mar [cited 2024 Jan 25]; 16(3): e0248916. Available from: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0248916. doi: 10.1371/journal.pone.0248916.
Hazarika M, Das S, Bhandari SS, Sharma P. The psychological impact of the COVID-19 pandemic and associated risk factors during the initial stage among the general population in India. Open J Psychiatry Allied Sci. [Internet]. 2021 Jan [cited 2024 Jan 25]; 12(1):31-35. doi: 10.5958/2394-2061.2021.00009.4.
Brunoni AR, Suen PJC, Bacchi PS, Razza LB, Klein I, Dos Santos LA, et al. Prevalence and risk factors of psychiatric symptoms and diagnoses before and during the COVID-19 pandemic: findings from the ELSA-Brasil COVID-19 mental health cohort. Psychol Med. [Internet] 2023 Jan [cited 2023 Dec 5]; 53(2):446-457. doi: 10.1017/S0033291721001719
Pan American Health Organization (PAHO). COVID-19 Recommended mental health and psychosocial support interventions (SMAPS) during the pandemic [Internet] 2020 [cited 2022 Jul 10]. Available from: https://iris.paho.org/bitstream/handle/10665.2/53017/OPASBRANMHMHCOVID-19200026_por.pdf?sequence=1&isAllowed=y
Inter-Agency Standing Committee (IASC). IASC Guidelines on mental health and psychosocial support in humanitarian emergencies. [Internet] 2007 [cited 2022 Jul 10]. Available from: https://interagencystandingcommittee.org/mental-health-and-psychosocial-support-emergency-settings-0/documents-public/iasc-guidelines-mental
Kunzler AM, Stoffers-Winterling J, Stoll M, Mancini A, Lehmann S, Blessin M, et al. Mental health and psychosocial support strategies in highly contagious emerging disease outbreaks of substantial public concern: A systematic scoping review. PLos ONE [Internet]. 2021 Feb [cited 2022 Jul 10];16(2):e0244748. Available from: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0244748 doi:10.1371/journal.pone.0244748
Muller AE, Hafstad EV, Himmels JPW, Smedslund G, Flottorp S, Stensland S, et al. The mental health impact of the covid-19 pandemic on healthcare workers, and interventions to help them: A rapid systematic review. Psychiatry Res. [Internet] 2020 Nov [cited 2022 Aug 8];293:113441. doi:10.1016/j.psychres.2020.113441
Yang X, Yang X, Kumar P, Cao B, Ma X, Li T. Social support and clinical improvement in COVID-19 positive patients in China. Nurs Outlook. [Internet] Nov-Dec 2020 [cited 2022 Aug 12];68(6):830-837. doi:10.1016/j.outlook.2020.08.008
Xiao H, Zhang Y, Kong D, Li S, Yang N. The Effects of Social Support on Sleep Quality of Medical Staff Treating Patients with Coronavirus Disease 2019 (COVID-19) in January and February 2020 in China. Med Sci Monit. [Internet] 2020 Mar [cited 2022 Aug 12];26:e923549. Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7075079/ doi:10.12659/MSM.923549
Antiporta DA, Bruni A. Emerging mental health challenges, strategies, and opportunities in the context of the Covid-19 pandemic: perspectives from South American decision-makers. Rev Panam Salud Publica [Internet] 2020 Nov [cited 2022 Aug 13];44:e154. Available from: https://iris.paho.org/bitstream/handle/10665.2/52997/v44e1542020.pdf?sequence=1&isAllowed=y doi: 10.26633/RPSP.2020.154
Gratzer D, Goldbloom D. Therapy and E-therapy-Preparing Future Psychiatrists in the Era of Apps and Chatbots. Acad Psychiatry [Internet] 2020 Apr [cited 2022 Aug 13];44(2):231-234. doi: 10.1007/s40596-019-01170-3.
Serrano-Ripoll MJ, Zamanillo-Campos R, Fiol-DeRoque MA, Castro A, Ricci-Cabello I. Impact of Smartphone App-Based Psychological Interventions for Reducing Depressive Symptoms in People With Depression: Systematic Literature Review and Meta-analysis of Randomized Controlled Trials. JMIR Mhealth Uhealth [Internet] 2022 Jan [cited 2022 Aug 13];10(1):e29621. Available from: https://mhealth.jmir.org/2022/1/e29621 doi:10.2196/29621
Bandelow B, Wedekind D. Internet psychotherapeutic interventions for anxiety disorders - a critical evaluation. BMC Psychiatry [Internet] 2022 June [cited 2022 Aug 13];22(1):441. doi:10.1186/s12888-022-04002-1
Egan SJ, McEvoy P, Wade TD, Ure S, Johnson AR, Greene D, et al. Unguided low intensity cognitive behaviour therapy for anxiety and depression during the COVID-19 pandemic: A randomised trial. Behav Res Ther. [Internet] 2021 Sept [cited 2024 Jan 25]; 144:103902. Available from: https://www.sciencedirect.com/science/article/pii/S0005796721001017 doi: 10.1016/j.brat.2021.103902
Hatta MH, Sidi H, Sharip S, Das S, Saini SM. The Role of Virtual Reality as a Psychological Intervention for Mental Health Disturbances during the COVID-19 Pandemic: A Narrative Review. Int J Environ Res Public Health [Internet] 2022 Feb [cited 2024 Feb 01]; 19(4):2390. Available from: https://www.mdpi.com/1660-4601/19/4/2390/htm doi: 10.3390/ijerph19042390
Brouzos A, Vassilopoulos SP, Baourda VC, Tassi C, Stavrou V, Kalliopi Moschou, et al. “Staying Home – Feeling Positive”: Effectiveness of an on-line positive psychology group intervention during the COVID-19 pandemic. Curr Psychol [Internet]. 2021 Mar [cited 2024 Feb]; 42(4):2749–61. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7980788/ doi: 10.1007/s12144-021-01613-x
Lucietto G, Pereira D, Sousa D, Souza D, Correia-Zanini, M, Scorsolini-Comin F. Online psychoeducation groups for mental health promotion: Perceptions of Brazilian university students. Couns Psychother Res. [Internet] 2023 Dec [cited 2024 Jan. 25]; 00:1-11. doi: 10.1002/capr.12736.
Margherita G, Benedetta Muzii, Alessia Caffieri, Adriana Di Francia, Somma B. “Isolated together”: online group treatments during the COVID-19 pandemic. A systematic review. Res Psychother. [Internet] 2022 Nov [cited 2024 Feb 3]; 25:365-85. doi: 10.4081/ripppo.2022.639
Malinauskas R, Malinauskiene V. Meta-Analysis of Psychological Interventions for Reducing Stress, Anxiety, and Depression among University Students during the COVID-19 Pandemic. Int J Environ Res Public Health [Internet] 2022 Jul [cited 2024 Jan 25]; 27;19(15):9199. doi: 10.3390/ijerph19159199.
Ye Z, Li W, Zhu R. Online psychosocial interventions for improving mental health in people during the COVID-19 pandemic: A systematic review and meta-analysis. J Affect Disord. [Internet] 2022 Nov [cited 2024 Jan 25]; 316:120-131. doi: 10.1016/j.jad.2022.08.023.
Doherty A, Benedetto V, Harris C, Boland P, Christian DL, Hill J, et al. The effectiveness of psychological support interventions for those exposed to mass infectious disease outbreaks: a systematic review. BMC Psychiatry [Internet] 2021 Nov [cited 2022 Aug 15];21(1):592. doi:10.1186/s12888-021-03602-7
Khademian F, Aslani A, Ravangard R, Bastani P, Nami M, Jafari P. Efficacy of a web application for stress management among Iranian college students during Covid-19 outbreak: a study protocol for randomized controlled trials. Trials [Internet] 2020 Dec [cited 2022 Aug 16];21(1):1023. doi:10.1186/s13063-020-04949-0
Dumarkaite A, Truskauskaite I, Andersson G, Jovarauskaite L, Jovaisiene I, Nomeikaite A, et al. The efficacy of the internet-based stress recovery intervention FOREST for nurses amid the COVID-19 pandemic: A randomized controlled trial. Int J Nurs Stud. [Internet] 2022 Nov [cited 2023 June 20];138:104408. doi: 10.1016/j.ijnurstu.2022.104408.
Meneses DA, Tavares JJC, Monteiro REM, Lopez LCS. Fenótipos digitais para mindfulness e ansiedade encontrados por aplicativo de smartphone. Saud Pesq. [Internet] 2023 Mar [cited 2024 Jan. 25];16(1):e-11196. Available from: https://periodicos.unicesumar.edu.br/index.php/saudpesq/article/view/11196/7284 doi: 10.17765/2176-9206.2023v16n1.e11196
Selltiz C, Wrightsman LS, Cook SW. Research methods on social relationships. New York: Holt, Rinehart and Winston; 1976.
Souza RC, Santos JE, Santos VTC, Silva AAF, Vasconcellos EA, Ambrósio PE et al. Psychosocial e-Therapies Project: Construction and strategies to promote mental health in times of pandemic Covid-19. Res Soc Dev [Internet] 2021 May [cited 2022 Aug 8];10(6):e20910615740. Available from: https://rsdjournal.org/index.php/rsd/article/view/15740/14027 doi: 10.33448/rsd-v10i6.15740
Vignola RCB. Depression, Anxiety and Stress Scale (DASS): adaptation and validation for Brazilian Portuguese [dissertation]. Santos, São Paulo: Universidade Federal de São Paulo, Instituto de Saúde e Sociedade; 2013. 80p.
Freitas ALP, Rodrigues SGA. Avaliação da confiabilidade de questionário: uma análise utilizando o coeficiente alfa de Cronbach. XII Simpósio de Engenharia de Produção; 2005 nov. 7-9; Bauru, São Paulo, BR. Anais. [cited 2024 Jan 25] Available from: https://simpep.feb.unesp.br/anais/anais_12/copiar.php?arquivo=Freitas_ALP_A%20avalia%E7%E3o%20da%20confiabilidade.pdf
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics [Internet] 1977 Mar [cited 2024 Jan 24];33(1):159-74. Available from: https://pubmed.ncbi.nlm.nih.gov/843571/
Elsaie ML, Hasan MS, Zaky MS, Hussein SM, Kadah AS, Omar AM. Implication of COVID-19 on the mental health of Egyptian dermatologists: A cross-sectional study. J Cosmet Dermatol. [Internet] 2021 Oct [cited 2024 Jan 25]; 20(10):3066-73. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8661565/ doi: 10.1111/jocd.14390
Bryant RA, Dawson KS, Keyan D, Azevedo S, Yadav S, Tran J et al. Effectiveness of a Videoconferencing-Delivered Psychological Intervention for Mental Health Problems during COVID-19: A Proof-of-Concept Randomized Clinical Trial. Psychother Psychosom [Internet]. 2022 Dec [cited 2023 Jan 3];91(1):63-72. doi:10.1159/000520283
Wang C, Pan R, Wan X, Tan Y, Xu L, Ho C et al. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int J Environ Res Public Health [Internet] 2020 Mar [cited 2022 Aug 10];17(5):1729. doi:10.3390/ijerph17051729
Duarte MQ, Santo MAS, Lima CP, Giordani JP, Trentini CM. COVID-19 and the impacts on mental health: a sample from Rio Grande do Sul, Brazil. Cien Saude Colet [Internet] 2020 Sept [cited 2022 Jan 5]. doi: 10.1590/1413-81232020259.16472020
Santamaría MD, Ozamiz-Etxebarria N, Rodríguez IR, Alboniga-Mayor JJ, Gorrotxategi MP. Psychological impact of Covid-19 on a sample of Spanish health professionals. Rev Psiquiatr Salud Ment (Engl Ed). [Internet] 2021 Apr-June [cited 2022 Jan 5];14(2):106-112. doi:10.1016/j.rpsm.2020.05.004
Baptista CJ, Martins AM, Escalda PMF. Factors associated with high mental health scores of university teachers during the COVID-19 pandemic. Saud Pesq. [Internet] 2023 Jan-Mar [cited 2024 Feb 3]; 16(1):e-11419. Available from: https://periodicos.unicesumar.edu.br/index.php/saudpesq/article/view/11419/7314 doi: 10.17765/2176-9206.2023v16n1.e11419
Silva AND, Guedes CR, Santos-Pinto CDB, Miranda ES, Ferreira LM, Vettore MV. Demographics, Socioeconomic Status, Social Distancing, Psychosocial Factors and Psychological Well-Being among Undergraduate Students during the Covid-19 Pandemic. Int J Environ Res Public Health [Internet] 2021 June 6 [cited 2022 Jan 6];18(14):7215. doi: 10.3390/ijerph18147215
Devkota HR, Sijali TR, Bogati R, Ahmad M, Shakya KL, Adhikary P. The impact of Covid-19 on mental health outcomes among hospital fever clinic attendants across Nepal: A cross-sectional study. PLos ONE [Internet] 2021 Mar [cited 2022 Aug 16];16(3):e0248684. Available from: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0248684 doi: 10.1371/journal.pone.0248684
Barros CSSC, Lima AJO, Souza RC. Welcome and promotion of well-being during the covid-19 pandemicin the on-line mode. CIS [Internet] 2021 Oct [cited 2022 Oct 2];21(4):211-24. doi: 10.53660/CONJ-181-510
Celuppi IC, Lima GS, Rossi E, Wazlawick RS, Dalmarco EM. Uma análise sobre o desenvolvimento de tecnologias digitais em saúde para o enfrentamento da COVID-19 no Brasil e no mundo. Cad Saude Publica [Internet]. 2021 Mar[cited 2022 Oct 2];37(3):e00243220. Available from: https://www.scielo.br/j/csp/a/rvdKVpTJq8PqTk5MgTYTz3x/# doi: 10.1590/0102-311X00243220
Oliveira P, Garcia R, Oliveira D, Batista D, Silva G, Bertolini S. Technological inclusion: effects on the mental health and quality of life of elders Saud Pesq. [Internet] 2023 Mar [cited 2024 Jan 25]; 16(1): e-10988: Available from: https://periodicos.unicesumar.edu.br/index.php/saudpesq/article/view/10988/7283 doi: 10.17765/2176-9206.2023v16n1.e10988
Downloads
Published
How to Cite
Issue
Section
License
A submissão de originais para a revista Saúde e Pesquisa implica na transferência da Carta Concessão de Direitos Autorais, pelos autores, dos direitos de publicação digital para a revista após serem informados do aceite de publicação.A Secretaria Editorial irá fornecer da um modelo de Carta de Concessão de Direitos Autorais, indicando o cumprimento integral de princípios éticos e legislação específica. Os direitos autorais dos artigos publicados nesta revista são de direito do autor, com direitos da revista sobre a primeira publicação. Os autores somente poderão utilizar os mesmos resultados em outras publicações, indicando claramente a revista Saúde e Pesquisa como o meio da publicação original. Em virtude de tratar-se de um periódico de acesso aberto, é permitido o uso gratuito dos artigos, principalmente em aplicações educacionais e científicas, desde que citada a fonte. A Saúde e Pesquisa adota a licença Creative Commons Attribution 4.0 International.
A revista se reserva o direito de efetuar, nos originais, alterações de ordem normativa, ortográfica e gramatical, com vistas a manter o padrão culto da língua e a credibilidade do veículo. Respeitará, no entanto, o estilo de escrever dos autores. Alterações, correções ou sugestões de ordem conceitual serão encaminhadas aos autores, quando necessário. Nesses casos, os artigos, depois de adequados, deverão ser submetidos a nova apreciação. As opiniões emitidas pelos autores dos artigos são de sua exclusiva responsabilidade.